|
|
Benjamin Franklin
|
Benjamin Franklin was able to retire from the printing business at the age of 42. His partners bought him out in eighteen yearly installments. In the Eighteenth century, it was unusual to live past the age of 60, so Ben felt pretty well fixed. Unfortunately for this planning, he lived to be 82, so when he did reach the age of 60 he was forced to look around for postmasterships and other ways to survive, for what proved to be 22 more years.
This is the other side of a coin; on one side is written, "Protect your family in case you die young". On the opposite side is written, "Be careful not to outlive your savings", relying on the old Quaker maxim that the best way to have enough--is to have a little too much. For centuries, life insurance was sold to people who mainly feared the first, commonest, possibility, but never completely addressed the opposite contingency, which was growing steadily commoner. Annuity insurance ordinarily is sold for a fixed number of years, so insurance commissioners ordinarily require what is most probable. Unfortunately, this response shifts the risk of guessing wrong onto the subscribers' shoulders. Since science has unexpectedly lengthened average life expectancy (by thirty years since 1900, or by five years in the last ten), experience rather like Ben Franklin's has become a commonplace, but rather poor business judgment. The business remains solvent only as long as the decision to drop the policy is later than the life expectancy.
|
|
Retirement Saving Debt
|
There may exist insurance policies to address this issue, but few companies offer it. We will briefly describe this sort of policy, in case it becomes more widely available, but it is primarily described here to illustrate the issues to consider. If you can get it for a reasonable price, or if you can get it at all, the outline of the policy would be to set a premium and promise to pay 6% for the rest of your life. Underneath the promise is the reality of paying 6% for eighteen years as a non-taxable return of principal. Following that, you don't need to get a postmastership, you are paid a taxable 6% until you die. Presumably, the insurance company has actuaries to help with the math, so the company makes money if you live less than your life expectancy, and loses money if you live longer. If life expectancy suddenly extends much longer (let's imagine a cure for cancer appears), the insurance company is going to go broke. That's why insurance commissioners are uncomfortable with the concept, even though it is obvious how desirable it might be. So that's why annuity insurance typically states a fixed number of guaranteed years and expects the subscriber to shoulder outlier risk.
Any insurance has an administrative cost, so everyone must consider some non-insurance solution to the whole problem. Therefore, we propose you re-examine the old saw about "never dip into principal". If you don't have enough money, you can't do very much except depending on the government, your family, or your fairy godmother to help you out, although it must be obvious that all Americans would be wise to consider retiring five or ten years later than they hoped. Very likely, the government is going to have a difficult time sustaining even the present tax exemption of retirement funds, medical insurance, and social security. Those are called entitlements, but if the government eventually can't afford them, it won't matter what you call them. If entitlements keep getting extended, we can expect our nation to resemble the ancient Chinese and Indian nations -- able to build palaces in their golden era, but eventually crumbling into a gigantic slum in centuries afterward. So please, if you are able to do it, try to keep gainfully employed for a few extra years. If you do it (and some people can't) you may be able to realize the American Dream.

|
|
Inheritance Tax
|
The traditional American dream was to accumulate enough money to live off the income from it indefinitely, never touching principal, and then exposing the principal to destructive estate taxes after you finally die. Unless you are unusually wealthy, there isn't much left for the next generation after estate and inheritance taxes and expenses. It's a little inefficient to accumulate more than you actually need, but the government gravitates toward the least painful methods of collecting taxes. By confiscating this safety surplus, however, it declares that "Every ship (generation) must sail on its own bottom." And therefore it must acknowledge responsibility for what inheritances ordinarily pay for, like charity and good works. But there remains a quirk to this.
If Ben Franklin's partners had arranged to invest the money until he needed it, they could at least have afforded to finance two or three extra years. After inflation and expenses have eaten away at your retirement income, your principal may not generate enough income to last forever, but it is still big enough to pay for several years of retirement, which may in fact be longer than you are destined to live. Remember two things: 1) a principal sum, big enough to support you indefinitely, must be roughly eighteen times your yearly expenses. If it is only big enough to support you for fifteen years, it will seem too small until you realize you are probably actually going to live, say, five years. And 2) as far as leaving an inheritance to your children is concerned, there is a realistic probability that the government will consume most of the estate before it ever gets to the kids. These fundamental truths are presently obscured by the Federal Reserve artificially forcing interest rates to less than 1%. But if you can just hold out for a few years, it seems entirely likely that interest rates will return to 6% (meaning your principal will once again produce eighteen equal installments). But such a return of interest rates to normal levels will force the government to pay a comparable amount as interest on its bond debts (meaning it will get hungrier to escalate your estate taxes.) This isn't nearly as satisfactory a solution to the life expectancy quandary as retiring five years later than you once expected to, but you can't say we didn't warn you.
And as for what happened to Ben Franklin, you can read his will. He died a very rich man as a result of shrewd investments, later in his life. Ben left eight or nine houses, several thousand acres in several states, a gold-handled cane, and a portrait of the King of France surrounded by hundreds of diamonds. But it would not seem wise for the rest of us to count on accumulating that much new wealth, after attaining the age of sixty. The way things are going, once you attain your life expectancy, everyone should have some non-insurance plan for supporting himself for two or three extra years.
It is misleading to make precise predictions, about almost anything, eighty or ninety years in advance. However, predicting the average of millions of people is more accurate than predicting any individual future, whereas mathematical principles like compound interest are precise, forever. But let it be clear; what follows is rounded off, estimated, and largely based on projecting past experience into future performance. You must do so, if you want to talk about it, at all.
Investments are more predictable than health costs. At 10% they will double in seven years; at 7%, doubling investments takes ten years. Ten in seven; seven in ten. From birth to age 91, there will be time for thirteen doublings of investments. At seven percent, only nine doublings. With a focus on health economics, Americans divide into four groups: children from birth to 26, working people from 26 to 65, retirees over 65, and poor people of any age. We assume only people from 26-65 are able to deposit money in Health Savings Accounts; children and poor people are dependent on working people to help them, while retirees must live on money they earned while they were 26-65. Businesses and governments are pass-throughs which sign checks, but in our way of thinking, only individuals make and spend money in the national accounting of it. These are the assumptions, please read them twice.
1. Investment predictions are based on Ibbottson's compilation of actual market performance since 1926 of all investments in all classes. It's safe to assume index funds, now available in the trillions of dollars, will follow Ibbottson's patterns for the next hundred years, only because they were remarkably steady during the last century. Two major depressions and a dozen minor ones, one World War and a dozen smaller ones, were unable to shake the long-term trends for more than a blip in the lines.No such prediction can be guaranteed, of course. Highly diversified, Index funds have management fees of about a tenth of a percent, making them steady passive investments for people who have little investment experience, and probably equalling performances of most people who do. Using Ibbottson's raw data, half the population will do better and half will do worse--by managing their own money, even with professional advice. But if everybody buys the index fund without advice, everybody will perform the same. Collectively, the average common stocks of "small" American corporations (but nevertheless greater than one billion dollars of market value each) achieved a ninety-year performance of 12.2%, which we here discount to 10% by using diversified ETF (index funds) of really big stocks with familiar names.
2. At present, the only realistic source of deposits into a Health Savings Account is by individual investors within the age group 26-65, except for investment income. Contributions made on behalf of children derive from money earned by working parents or by -- somebody else aged 26-65. Retirees invest, but the core of what they invest was earned earlier, again 26-65. We ignore exceptional cases. The population 26-65 supports their own costs and those of everybody else. Nevertheless, it is impossible to make precise predictions about the time and amount of shortfalls in individual Accounts when sudden withdrawals must be anticipated. For the most part, transfers are made from accounts in surplus to accounts in deficit, but particularly during the phase-in period, supplements may be necessary. However, everybody's Health Savings Account is a separate piece of property and not a pool. This difficulty is managed by slightly overfunding everything to keep transfers to a minimum, and pooling these surplus amounts by agreement to reimburse them at some later time for some specific purpose. Furthermore, the principle is announced in advance that if shortfalls are unavoidable, the accounts to be billed for it are to be limited to the working-age group from 26 to 65. The ultimate fallback is the full faith and credit of the taxing power of the U.S. Government; but we hope to avoid using it except in dire emergencies like a national nuclear attack or something else of this order of severity, eventually establishing a reputation of a self-funding program. Within that program, the real fallback is to the 26-65 generation who are earning a living. They are expected to care for their children, and aging parents, but by individual agreement. Since the plan is to stop collecting 6.5% payroll deductions from this age group, and anticipated deficits are of the nature of 0.5% of income, assessments should be comfortably met, although it is too much to expect them to be cheerfully met. A whole chapter is later devoted to this sensitive topic.
2.5 Transfers are necessary, however. Because of the security risk, it is probably wise to introduce the extra step of transfer into and out of an insurance or insurance-like pool, so that transfers between Health Savings Accounts can be performed by a tightly controlled security organization which maintains permanent transaction records as its main or only function. Pooling would actually ease the accounting burden of linking every account in surplus with every account which runs a temporary deficit when actually it is only necessary to account for the balances between individual accounts and the pool. If newborns have individual accounts, they will have to be linked to their parents or guardians, and perhaps transferred from their parents' accounts at age 26. Although making health insurance a personal rather than a community activity is a step forward, there will be much occasion for reducing individual volatility while the accounts are still too small to provide their own liquidity reserves. This is also the place to put subsidies for the poor, and payroll tax assessments on the 26-65 age group, replacing the 6.5% payroll tax for Medicare pre-payment, which has been eliminated out of consideration for dropping later Medicare coverage. After the transition phase is complete, the pool will be less necessary, but it may take decades before money spent on obstetrics comfortably matches up with money pre-funded for cancers and strokes.
3. Medical costs essentially do not matter for lifetime plan design, since this is "found money". Rising costs are of course the main concern, and of course, we should pay all of them, but not necessarily by investment income, entirely. We strive to generate as much new revenue as possible and are confident it will raise appreciably more than the present system. If more is needed, additional sources must be sought. It might, if all went as planned, generate half of the cost of healthcare in the far future. But it will never seem like that much, because we are already outspending our revenue, and borrowing the shortfall. Only after our books balance on a current basis, will the public notice any difference. Congress will notice it sooner and be tempted to spend it. If it generates more than we need for healthcare, then if we are wise we really should spend the surplus on retirement costs for an aging population.
However, the outlines of what is possible can be made out. Likely, future medical costs for younger individuals under the age of 65 should remain constant, or even decline in the future. However, medical costs of the elderly are assumed to rise in the future, as people live longer and get more expensive chronic diseases. CMS says 5% of the elderly generate 50% of costs for their age group. Conditions related to obesity are a new source of such costs, while Managed Care has had no effect. Exceptions will appear but predicted cost curves seem likely to assume the shape of a dumbbell, bulging at the ends, but shrinking in the middle. Since working cash for inter-person transfers and unexpected illness are laid on the working age group, it is a lucky happenstance that future predictions almost always show a dumbbell or wasp-waist shape to the cost curve, making it possible to design budget shortfall levies to concentrate on this level. The biggest threat to future healthcare financing may well lie in the likelihood that people who now die at the age of 60 will live to be 85, and be afflicted with the same high expenses as we now see in people aged 85. If present trends continue, the rising costs after age 85 contain a mixture of falling sickness costs, hidden within rising domiciliary costs, or nursing home costs, which possibly belong in a different budget. This outcome seems more likely that the present rate of longevity extension, which is more likely to level off. However, the original point is the strongest on: it is a mistake to pretend to predict a future which cannot be predicted.
4. We assume average health costs for a lifetime to be $300,000, based on a Blue Cross of Michigan study, confirmed by AHRQ and CMS to be of that general magnitude. It is a critical number since it is the burden workers age 26-65 must carry for the whole medical system at every age--averaging $7800 per year apiece for the working person. It is important to know how it is calculated, to understand what it means -- and what it doesn't.
Calculated as described, the $7800 pays for one working person, plus averaged contributions for dependents and charity obligations. Because of cost-shifting, the proportion of redistribution is unclear. But, remember, these are lifetime costs, using current prices. If costs remain otherwise identical, a 3% inflation rate means the answer, calculated the same way next year, will be $309,000. This point is made to convince the reader, that even if we do not know the precise costs, we can be fairly sure that costs will soon outrun our ability to cope with them.
In order to include present costs and present practices, a hypothetical person is constructed from current costs at each level, reassembled in order to reflect current costs for current treatments, as if they all occurred in the year of death. It, therefore, includes 3% inflation over the time span from birth to each particular age. The modest costs of childhood are thus inflated the most, while the expensive last year of life is not inflated at all. Since it will be adjusted in the next paragraph, it is probably not a serious error.
Predicted Future Healthcare Costs. If the $300,000 we spent on each person's health in the last 90 years should merely increase at 3% inflation, lifetime costs will become $4.5 million, 91 years from now. That's sobering enough. But if medical costs increase as much as they actually did in the past century, lifetime costs will come to an unthinkable $1.5 billion dollars a person. Therefore, we accept the present hypothetical lifetime cost, including inflation, to have been $300,000, and assuming no change other than 3% inflation, will be $4.5 million, 91 years from now.
Nevertheless, we know in retrospect that a solitary deposit of $55 in 1926 at the 10% rates which actually prevailed last century, would have kept even with it without later additions. Today, to keep up with the costs of a newborn great-grandchild could apparently be accomplished with a deposit of $796, over twelve times as much. It's still an achievable goal, but it's drawing away from us. Remember, $800 will only pay for present prices, plus 3% inflation. Unlike the last century, the next century cannot add thirty years to life expectancy, or eliminate thirty diseases. In fact, only five remaining diseases account for half the cost, and life expectancy has no room left to increase by another thirty-year extension. The medical profession has the scientific tools to make it work, provided the financial and political professions create the right environment. The present prospects are for science to deflate disease costs in every age group except the oldest, but to quantify is impossible. Since 1913 when the Federal Reserve was founded, a dollar then is worth a penny, now. The medical profession can't help with inflation. Perhaps no one can, but at least a monitor exists to make mid-course corrections of the currency.
More than that, notice the difference between $300,000 and $796. The difference, although roughly estimated, suggests the savings possible by switching to lifetime costs, and investing the difference between "whole life" and "pay as you go" annual payments. It is unnecessary to come even close to actual costs to see the savings from financing the medical system longitudinally, outstripping anything imaginable in extra administrative costs, or price escalation from moral hazard. Cut it in half, or take only a tenth, the savings are so appreciable you begin to wonder if they might upset the stock market. There are even safeguards from miscalculation, remaining inherent in other approaches to cutting the cost of medical care.
For example, we fervently hope, but make no assumption in the example, for an extension of working life, both down and up, to 24-75. That is, we favor a reduction of the two great vacation periods in American life, by a parallel extension of the lifetime of significant work. We recognize most Americans do not agree, and in a democracy that's how decisions are made. But this safety valve remains available to those with bad luck or bad timing; it's how you recover your finances if they have slipped along the way.
Let's cut wasteful practices, particularly the habit our government has of making hospitals into welfare programs, or our insurance administrators have for making them into banana republics, and the habit the public has of wanting everything for free. Let's structure costs in such a way that if an individual doesn't overspend for healthcare, the money saved gets applied to better retirement. It gives the individual some skin in the game, which is the essence of bringing costs down by competition.
Right now, however, it is necessary to examine how we might extract the savings from Health Savings Accounts, gradually transitioning from one-year term to whole life with investment, without upsetting the system. And examining what useful things might be done with a cash windfall before too many extra noses push into the trough. After all, you cannot spend the money after you are dead.
Let's start backward from an assumed guess of $300,000 average lifetime expense, from the viewpoint of someone aged 90, which is also only guessed-at future longevity, to the day of death. To have $300,000 at age 90, you must have $30-40,000 set aside at age 65 in index funds. Remember, in the elderly, we are talking about the period of greatest health costs by present projections, in an age group where few people are working and thus must entirely depend on investments and pensions. It can be done but it's a stretch. In many ways, the greatest obstacle would be the mindset of elderly people themselves. We are talking about buying common stock for elderly people, who must overcome the main reason they buy high and sell low. Left to themselves, they will lean toward the safety of low-yielding bonds.
We have repeatedly alluded to The Monitoring System, which will take time and experience to design. Whether the monitor resides within the Treasury, the Department of Health or some independent agency is a political question that others probably feel they have a better right to decide. Such an agency might have many functions, but since it must have the power to make myriads of mid-course adjustments, it probably requires a self-balancing oversight board like that designed for the Federal Reserve, and we favor that approach. At least once a year, that monitoring body will have to recalculate the estimates of the emerging trend of the balances between costs and revenues, and the distribution of the balances among each yearly cohort from birth to age 91.
Those yearly recalculations would set the price of entry into the system for latecomers, calculating what it would cost to make up for failing to pay for it all at birth. And if the system makes a revision for new information about trends in motion, everybody will in a sense be a newcomer, subject to a late deposit levy. And since the working adults 26-65 will be picking up the extra costs for birth to 26, plus charity cases at all ages, there will have to be secondary and tertiary adjustments in the levy. Furthermore, there may be a recalculation of the cost of a particular age cohort for current medical expenses, and that will have to be set as an additional deposit required for that age cohort. Meanwhile, the investment managers will report on how close they came to their target, and further adjustments made. The Federal Reserve will make a report on current inflation rates, leading to more adjustments. The ultimate goal is to set a price for late entry at each year, so that continuing future income distributions will be equal, for current entrants, as for those who made a lump-sum investment at birth. This monitoring system will also be responsible for smoothing out short-term volatility, as in an influenza epidemic, and possibly long-term readjustments of internal lending and borrowing which were not anticipated at the outset of the program.
The Elderly Investor. Although the Libertarian view is that people ought to be able to do what they please with their own money, this is one case where it probably would be advisable to mandate the pooling of investments, in spite of the obvious introduction of political risk. The argument runs: it might be possible for most people to save $30-40,000 by any number of ways before the age of 65. But after 65 it becomes a little unwise for a growth fund to place trust in the investment judgment of a class of people who rightly prize security overgrowth. They will predictably have a very hard time shaking the perceptions of their age group. On the other hand, if there is ever a chance people will accumulate $45,000 in savings, it would be at the time they stop working. Let's hurry on; our present purpose is to illustrate the principle we are driving at.
Working people 26-65. Between the time they get their first job and the time they retire, working people have children, send them to college, buy a house, and try to come up in life a little. They get dozens of claims for their support, so in our example, to have perhaps $35,000 to surrender at age 65, using our system they might alternatively have to have $500 available at age 27, from Santa Claus. And then let it grow, untouched, to the next goal of $35,000 when they reach 65. That sounds easy, but it often has its problems. If somebody, say their parents, gives them the $500 as a present, it's all pretty easy. But if they have to work for it, then somebody has to give them $35 at birth, because the daisy chain is connected from start to finish. That's right, $35 turns all the way into $300,000 at age 90 if each step is coordinated. It pays for an entire lifetime of health costs. But it doesn't need to. If just about everything goes wrong, a quarter of that would still amount to a big chunk of money. Are you going to tell me no one could afford to give $7 to a newborn? There's no rule against making a partial contribution to your own care. There are practical problems to be addressed, but the power of compound interest isn't one of them. In fact, you might easily find that no investment house would accept a $7 deposit for a 90-year forward account.
Children. After the elderly, the second subsidized group is composed of children, including obstetrics and pregnancy. There is overlap here between child and two parents, and for conceptual purposes, there is nothing to do but be arbitrary. The addition of 26 years of compounding is too tempting to quibble about ambiguities, which might be solved by giving it to any of them, or to all three. That heightens the unfairness to those who do not have children, but it also creates an incentive for the mother to have her first child younger. Medically, that would be a desirable thing. Our society, perhaps even our biology, has created a tradition that the parents subsidize the health costs of children. The Health Savings Account system formalizes that tradition or at least does not conflict with it. For the surprisingly small amount of one single payment of $150 at birth, the child would have $40,000 at age 65, assuming a 10% investment return. Investment advisors might rebel at their costs for accepting amounts that small, but a single-payment zero-coupon bond or credit might be created. That would ease the mechanics, as well as reduce the outcry against federal subsidy to people who might be indigent when the child is born, but are far from it later in life. The disadvantage is a bond makes no provision for the health care of children even though it pays for it, so some patchwork is still needed. A birth deposit of $150 would be worth about $2000 at age 26, and average childhood medical costs might be somewhat greater, so a transfer of ownership could imply a net liability.
The Poor. The third and last category of subsidized people consists of those who are both poor and sick at the same time. Unfortunately, we have tried and rejected two methods of dealing with their problem. The first was defined by the original Good Samaritan: "Take care of him, and I will repay thee." And the second method was almshouses, now a relic of the past. The disadvantages of both approaches are now obvious. The third method was to eliminate poverty, which has worked pretty well. Fifty years ago, sixty percent of the hospital beds in Philadelphia were "ward" beds. Nowadays, there are few enough of them to scatter among paying patients. But the disadvantage soon appeared that the public became determined to prevent the inevitable rationing from spilling over to more fortunate components of society, in an era when hospitals are fearful of discrimination. Mindful of the long history of charity for the sick poor, and the spotty history of using government to cover the costs, we propose that governmental charity be paid out of the pool for inter-account transfers. That preserves an independent audit of just how much is paid by whom, and it is linked to an assessment process on people who must pay the bill. That will not prevent government from discounting its contribution, as it does not prevent Medicaid from discounting hospital bills. But it widens the audience who are instantly aware of it, all of whom will be heard from in the November elections. Individuals are compassionate, governments only pretend to be. You would almost have to say it is the one remaining good feature of having a King -- to symbolize the nation's simultaneous aspirations, of opulence and compassion.
Since America has rejected the obvious approaches to caring for the sick poor (almshouses and blank checks), our institutions are in some disarray. We even seem to be rejecting a mixture of the two, which was the hospital reaction to the 1965 entitlements. Until we identify and concentrate the sick poor in some way, we cannot even measure the size of the problem. But at least concentrating the rest of the population's sickness on paper allows us to measure their cost and (by subtraction) estimate a health budget for the sick poor. It will inevitably cost more than average, and result in worse outcomes. But only after we measure it, can we even decide how much we can afford.
What you have, including the three demographic subsidies, is what it seems to cost working people in today's environment to care for themselves and their obligations. It's distributed over forty years of working, but not everybody works that whole period of time. If you wish, you can contribute $100 a year from age 25-65, a surprisingly small amount which after compounding at 10% should pay the lifetime costs of one person (yourself). Calling it $150 to be safe, it is no more than a tenth of what most people suppose they pay for annual health insurance. Therefore, it is safe to suppose a family of four could afford to pay for ten poor people (in addition to themselves) at the cost they are already spending. Remember please, our goal is not to pay for all health care to the last penny. Our goal is to devise ways to pay for as big a chunk of it as we can.
And by the way, devising some method to get the latent money out of these accounts for medical care, since $300,000 does no good in a frozen account of somebody aged ninety. Please read on.
One secret of success for Classical Health Savings Accounts lies in recognizing a single approach is inadequate; at least two approaches are required. Catastrophic health insurance spreads big risks (mainly hospitalizations), while tax-free accounts promote more frugal spending for small ones (mainly ambulatory care). Combined in an HSA, they do what neither does alone, by covering overlaps. Now I contend, six principles in combination can create even greater savings, when separately they might create more confusion.
1. Redesign Insurance. Health insurance has traditionally been upside down. Starting with "first dollar" coverage, really sick people feared bankruptcy when medical costs outran policy limits for the last dollar. Obviously, it would be better to ensure big catastrophes first, skipping small ones if funds run out. If we must have mandatory health insurance, the thought ran, let it be the high-deductible catastrophic variety, with out-of-pocket limits protecting outliers. To a certain extent, the Affordable Care Act moved in that direction, possibly opening room for compromise. Deductibles should be high, but co-payments are useless and should be eliminated. Subsidies should subsidize people, not specific programs, and should avoid taxing the same program they are supporting.
2. Indirect Transfers Between Age Groups. Working-age people largely finance the health system but most don't get sick themselves, whereas sick people are mostly retired and on Medicare. That makes young people restless, while Medicare breaks the national budget with a 50% subsidy. (It's largely accomplished through bond-loans from foreign countries, like China.) The age-related funds' transfer is desirable but is now largely left to hospital cost-shifting. The cost could be lessened by letting the worker keep health money in his HSA, earn interest, and spend it on himself when he ages. 2b. Furthermore, I propose we shift the cost of the two most expensive medical years of life to individual escrow funds during the period of investment. To be specific, shift the cost of the first and last years of life from coverage by catastrophic health insurance and Medicare -- to repaying average national cost (reported by Medicare) back to the insurers who originally paid the bills. That's technically known as first and last years of life reinsurance.
3. Funds Creation. How might we pay for this transfer? Well, in the first place, living people are assumed to have somehow already paid for their birth year. It will be forty more years before new ones are even half-way phased in. Even terminal care costs will not level out until life expectancy stops lengthening. Revenue, on the other hand, could commence immediately. The hard part of revenue production lies in fixing "agency" failures. That is, avoiding spending it in the meantime, and keeping middle-men from poaching on it. I propose individual escrow accounts are preferable to agency management by either government or private sector financial institutions. Saving for your own rainy day is much more palatable than taxing for transfers between demographic groups. The cost of passive investment in index funds is small, and long-run gross returns approach 11%, or 7% net. But middle-man costs are often too high. Considering the trillions in index fund potential, these inert investments might even be considered for a substitute currency standard. Gold is too rigid, government judgment always proves too inflationary.
4. Compounding. Meanwhile, it helps to recall what the Ancient Greeks knew about compound interest. Money at 7% doubles in ten years, and therefore with life expectancy now at 84, can expect to double more than eight times. 2,4,8,16,32,64,128,256, (512- 1024). Unfortunately, the rounding errors also get compounded. Therefore, although the general concept is unchanged, one dollar at birth actually grows to about $289 at the average time of death by present expectations of it. By that time, life expectancy will likely grow by unpredictable amounts, so it might actually transform one dollar into $500 if inflation is held to no more than 3% -- or to some other value, more or less. The main hope for price stability lies, not so much with the Federal Reserve, as in medical science reducing the burden of disease and increasing the productivity of the delivery system. I feel confident last-year costs can be covered, either by patient contribution or by government subsidy, if -- transition costs are absorbed over the first decade or so, if the Federal Reserve can successfully hold inflation below 3%, and if medical science can cure one or two major diseases inexpensively in the next fifty years. Otherwise, this could merely be a proposal for generating tons of new revenue but would fall short of paying for all the healthcare affected. Even covering by only 10% would produce staggering sums, however.
Let me remind you, those extrapolations are for only one dollar invested. More specifically, the goal of the proposal is to pay for the last year of life by some variant of one-time investing of $150 at birth, possibly even as much as $50 per year. This should be enough to relieve the debt pressure on Medicare and to reduce the cost of catastrophic care for the rest of the population considerably. It's still much less costly than continuing the present approach.
5. Adding a Generation to the Family. To include the cost of children, we propose increasing the $150 at birth to $200 (potentially, $25 a year) and transferring the resulting surplus, from the grandparent's "bequest" to the Health Savings Account of no more than one grandchild at birth, thereby adding 21 years of compounding, broadening the scope to the first 21 years of life, and further reducing the premiums of catastrophic coverage for the rest of the population. Child-care costs are far more significant than they sound, and all health care plans have faltered on them. It is nearly impossible to refund the day you are born, particularly when the responsible parents are young and financially insecure, facing the cost of an automobile, a house, college education, and another child. For a remarkably small dollar cost, compound interest can greatly relieve this social environment, and therefore I advocate the small additional cost of extending the first year of life to the first twenty-one of them. And funding them via the grandpa route.
6. Tax Equity. Additional required regulations are more or less self-evident, but the most important one would be to permit paying for catastrophic insurance premiums by the Health Savings Account itself, thereby creating tax exemption equivalent to employer-based insurance.
(7) The overall result presented here is to shift the costs of children up to age 21, plus the last year of life, to a longer compounding period and to their ultimate source, which is working people from age 22-66. It adds a major source of revenue through extended compounding, and it does this at the reinsurance level, mostly insurance company to an insurance company. By shifting these costs, other programs cost less, and cost-shifting at the hospital level should greatly be reduced. As scientific research reduces costs, Medicare is destined to shrink, so its revenue can gradually be shifted to retirement income. That isn't exactly privatization, although politics may describe it so. In the far, far, future, health care might reduce along with a designated pathway to nothing but the first and last years of life. Or, the concept may be dismantled and pieces of it used in other ways.
(8) The alternative for tax equity is much more drastic -- of reducing corporate tax rates, sufficiently to compensate companies for losing their existing tax preference. For years, reformers have advocated tax equalization by eliminating the tax deduction for employees. It hasn't been successful, so now we advocate equalization first, reduction later. If that is blocked, there is no choice but to lower corporate taxes, paradoxically the source of the problem.
America only needs to price its sovereign bonds to a small spread below the prices of its many component corporate bonds, whereas the common market drives multiple sovereign nations to compete in bond prices. Consequently, half of the member nations will oppose consolidation. because bond rates and prices go in opposite directions. The economically stronger nations, no matter who they happen to be, will always have an incentive to oppose bond consolidation because they see it as the richer nations subsidizing the poorer ones when they wanted to believe their success was their own ingenuity and hard work. When survivors of a previous war are still alive it gets even harder to raise your own costs on behalf of a former enemy. The poorer nations, for their part, pay dearly for the opportunity to inflate away government expenditures. Texas surely nursed feelings of this sort in 1913 when the Federal Reserve demanded national bond rates. But only the ignorant ones feel that way, today. New York is constantly looking for ways to escape subsidizing Alabama, but eventually, the tide will turn. New York and California are eternally bemoaning their high taxes, so there is probably an upper bound to what will work. Meanwhile, stocks in a panic fall further than they should have because they had risen too high.
There are no perfect alternatives, but the volatile nature of interest rates creates opportunities to introduce variable mixtures of active and passive bond pricing, depending on circumstances, as an outgrowth of the obvious need to introduce a new currency gradually. The American experience of having state and federal bond systems coexist may well provide useful guidance, and in any event, shows unification can be accomplished.
The price of borrowed money includes a provision to pay for defaults on the loan. That is, the interest rate demanded includes a default provision assessed by the banker against what he thinks is the risk of bankruptcy. Since he wouldn't make the loan if he thought the risk was high, he insures a little more accuracy by assigning a general rate of risk for the class of debtor. But what of the creditor who wouldn't suffer much, no matter what the risk of default? Or who ignores the risk of default because he sees very little? That man would have no interest in supporting loans, except to obtain an adequate rate of return; a pure investor, who has the money and is looking for a place to earn a return. If you don't give him a fair return, he will simply pass bonds by, and invest in something else. If the banker feels the risk is greater than the offered return, he too will let the opportunity pass. The consequence is for a fair price to emerge from the marketplace for bonds. The debtor may cry and protest, talking about the unfairness of it all, and telling his wife that bankers are a greedy bunch of knaves. But in a modern bank, he would merely be offered a Kleenex for his performance. There are just times when loans are expensive, and this particular debtor has encountered one. Sometimes, a disappointed debtor visits his congressman, and sometimes the law is adjusted for him to borrow at a substandard rate. James Madison felt that debtors would always outnumber bankers, so there would be a tendency for interest rates to creep upward in a voting republic. Consequently, a mixture of strategies is employed to suppress interest rates. Sometimes the government subsidizes non-market prices, sometimes the risk of default cost is buried in the overall interest rate, sometimes the bank subsidizes the cost out of more obscure profits, usually by raising the rates for wealthier clients if they are numerous. If these simple strategies go on long enough, the default occurs and its cost is assessed as taxes from the bankruptcy courts. In a modern bankruptcy, the defaulted debtor may be entirely stripped of his other assets. If that's not sufficient to cover the loss, either the banking system collapses, or the government does.
There's another big player in this game: insurance companies. Insurance companies buy lots of bonds, trying to match their interest cost with their other expenses, notably their insurance liabilities. If the insurance commissioner of the state permits it, they may even issue some bonds to cover a shortfall. In recent years, they usually buy stock equities, and if they overdo it, the stock market may get them. The crooks in this business take in the premiums in the early years, and sell the company as the aging liabilities grow older, particularly if the Insurance Commissioner is friendly. Fortunately for them, the population has added thirty years to the life expectancies of their clients, so they have not had to resort to any of these strategies as much as they originally did. Insurance companies have been very profitable, and so bond rates have developed a great deal of slack. Whether they take advantage of their opportunities is not for me to say, but it would not be surprising if bond prices, hence bankruptcy laxness, have been both profitable and slack. The two are huge pools of money, operating in largely independent markets, which can operate comfortably and separately, for long periods of time. The last two stock market crashes have been real estate collapses, and real estate is all about mortgages, banks, and interest rates. And the Federal Reserve has responded to both crashes by artificially manipulating mortgages, banks and interest rates.

 Originally the "lower counties" of Pennsylvania, and thus one of three Quaker colonies founded by William Penn, Delaware has developed its own set of traditions and history.
Originally the "lower counties" of Pennsylvania, and thus one of three Quaker colonies founded by William Penn, Delaware has developed its own set of traditions and history.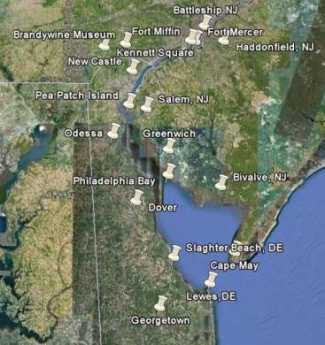 Start in Philadelphia, take two days to tour around Delaware Bay. Down the New Jersey side to Cape May, ferry over to Lewes, tour up to Dover and New Castle, visit Winterthur, Longwood Gardens, Brandywine Battlefield and art museum, then back to Philadelphia. Try it!
Start in Philadelphia, take two days to tour around Delaware Bay. Down the New Jersey side to Cape May, ferry over to Lewes, tour up to Dover and New Castle, visit Winterthur, Longwood Gardens, Brandywine Battlefield and art museum, then back to Philadelphia. Try it! Millions of eye patients have been asked to read the passage from Franklin's autobiography, "I walked up Market Street, etc." which is commonly printed on eye-test cards. Here's your chance to do it.
Millions of eye patients have been asked to read the passage from Franklin's autobiography, "I walked up Market Street, etc." which is commonly printed on eye-test cards. Here's your chance to do it. In 1751, the Pennsylvania Hospital at 8th and Spruce was 'way out in the country. Now it is in the center of a city, but the area still remains dominated by medical institutions.
In 1751, the Pennsylvania Hospital at 8th and Spruce was 'way out in the country. Now it is in the center of a city, but the area still remains dominated by medical institutions. Grievances provoking the American Revolutionary War left many Philadelphians unprovoked. Loyalists often fled to Canada, especially Kingston, Ontario. Decades later the flow of dissidents reversed, Canadian anti-royalists taking refuge south of the border.
Grievances provoking the American Revolutionary War left many Philadelphians unprovoked. Loyalists often fled to Canada, especially Kingston, Ontario. Decades later the flow of dissidents reversed, Canadian anti-royalists taking refuge south of the border.